Cells are the basic independent units of life. Single-celled organisms display an astounding array of specialization and structure, enabling them to individually meet life's challenges.
Within the context of a body, however, cells rarely display autonomy, but continually interact with other cells and the extracellular matrix that surrounds and physically supports them. The cells of most animals are so highly specialized in form and function that they have lost the potential for independent living, and are often clustered into clearly identifiable masses. Cell clusters that perform similar functions are referred to as tissues.
 |
 |
 |
 |
 |
 |
 |
 |
 |
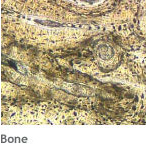
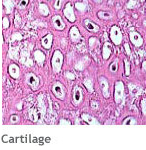
The structural and functional differences exhibited by tissues are direct consequences of both cellular and extracellular phenomena. All cells within tissues are separated and interlinked by an extracellular matrix (ECM) secreted by those cells. This ECM varies in composition from one tissue to another. Consistency may vary from a liquid (blood) to semisolid (cartilage) to solid (bone). The combination of cell activity and surrounding matrix is capable of producing a variety of tissue properties, ranging from transporting substances to serving as a protective scaffold.
There are four general classifications of human tissues, based on structure and function.
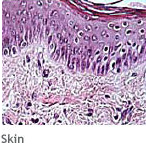
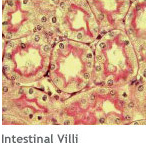
- Epithelial tissues cover the body and organ surfaces; line the body and cavities and form glands.
- Connective tissues bind, support and protect body parts.
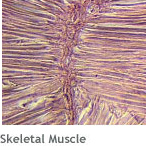
- Muscle tissues contract to produce movement.
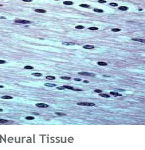
- Neural tissues initiate and transmit nerve impulses from one body part to another.
Over the last two decades, significant advances in understanding within the fields of cell biology, biophysics and biochemistry have yielded a greater understanding of the characteristics of living tissues. This insight into their structure and behavior has enabled researchers to plan the design and creation of new living tissues and organs to replace those that are diseased or missing.
Although scientists can trace the origins of tissues and characterize their functions, many questions remain.
- How do cells know into what tissue they are to mature?
- How do tissues maintain their structural and functional identity?
- How do tissues coordinate their activities within the body?
- Why can some tissues regenerate and not others?
- Why can human fetuses regenerate limbs?
- Why do newborn babies rarely scar?
- Genes are segments of DNA that code for particular molecules (usually proteins) and provide a structure or a particular metabolic activity for the cell. Genes determine the morphology and function of a cell or tissue. (The question of what alters the expression of genes in cells or tissues is one that scientists continue to study.)
- Growth Factors are regulatory molecules that affect cell and tissue function by influencing the differentiation of cells, altering their biochemical activity, and regulating their rate of proliferation. Cells within the same tissue signal each other by secreting growth factors while tissues in the body use them to communicate with each other as well. Over 100 growth factors have already been identified, and scientists have made great strides in understanding their functions. In a major breakthrough, scientists discovered that abnormal cell signaling is one of the defining characteristics of cancer.
Major challenges confront all tissue engineers, including enervating and vascularizing tissues so that, once developed, they remain fully functional.
Scientists employ these regulatory molecules to guide the development of engineered tissues. A common method involves the development of a biodegradable "scaffold", one that can temporarily exist in the body, resist any physiologic stress, and safely biodegrade over time. This scaffold is seeded with a cell population that is capable of proliferating and differentiating into a precise type of tissue. The seeded cells, in combination with existing bodily cells, eventually construct and maintain a new extracellular matrix, resulting in functional tissue. Tissue engineers have used this strategy to successfully create replacement tissues ranging from cartilage to bone to heart valves.
Obviously, the more complex the tissue, the more involved are the processes to create it in the laboratory. Whole organs, such as liver or heart, require vast amounts of resources (expertise, time and money) to develop. And major challenges confront all tissue engineers, including enervating and vascularizing tissues so that, once developed, they remain fully functional.
The Role of Stem Cells
Not all cells are easily influenced by growth factors. Many cells are too differentiated - that is, they are too specialized. For this reason, the medical research community has invested heavily in the search for "primordial" cells that have the proliferation and differentiation properties necessary to regenerate various tissue types. These immature, unspecialized cells, called stem cells, have retained their ability to enter particular developmental pathways, yielding specific types of differentiated cell populations.
A major goal of cellular therapy research is to identify and isolate these stem cells. It is hoped that, given precise biological cues, such as growth factors, these cells can be manipulated to created healthy tissue. For example, neuronal stem cells may be capable of restoring new brain cells in patients with a disease such as Alzheimer's or in trauma patients who have lost brain tissue.
After the addition of regulatory molecules to the damaged site, a limb bud may soon appear, followed by more extensive growth and tissue development.
Stem cells represent enormous potential for treatment and cure of medical conditions ranging from diabetes to paralysis. Scientists can envision a time when the biological basis of cellular differentiation will be well understood and the manipulation of tissues within the body will be possible without the introduction of an artificial construct, such as a scaffold. Instead, biologists will induce the repair, replacement or enhanced function of a tissue with a combination of the appropriate regulatory molecules. In a dramatic scenario, a person who has just lost a limb may be a candidate for this advanced technology. After the addition of regulatory molecules to the damaged site, a limb bud may soon appear, followed by more extensive growth and tissue development.
This scenario might be dismissed as science fiction but for the fact that other complex, vertebrate animals manage to re-grow limbs routinely and without the aid of any technology. Salamanders, for example, are well able to re-grow a severed limb and they possess all the same cell and tissue types as humans. This simple fact evokes great optimism for those in the biomedical community for it suggests that with an increased understanding of physiology and biological processes we might one day be able to manipulate tissues with relative ease. Until that time, scientists continue to pursue the near-term goals of tissues created with scaffolds and cell seeding.